Rehabilitation Aid
Rehabilitation aids are devices or equipment designed to assist individuals in their recovery process following an injury, surgery, or illness. These aids help improve mobility, strength, flexibility, and overall functionality. Here are some common types of rehabilitation aids:
Exercise Equipment: Various exercise tools and machines can aid in rehabilitation. These include resistance bands, therapy balls, balance boards, and pedal exercisers. They help strengthen muscles, improve range of motion, and enhance balance and coordination.
Walking Aids: As mentioned earlier, walking aids like canes, crutches, walkers, and knee walkers/scooters can assist individuals in regaining mobility during their rehabilitation journey.
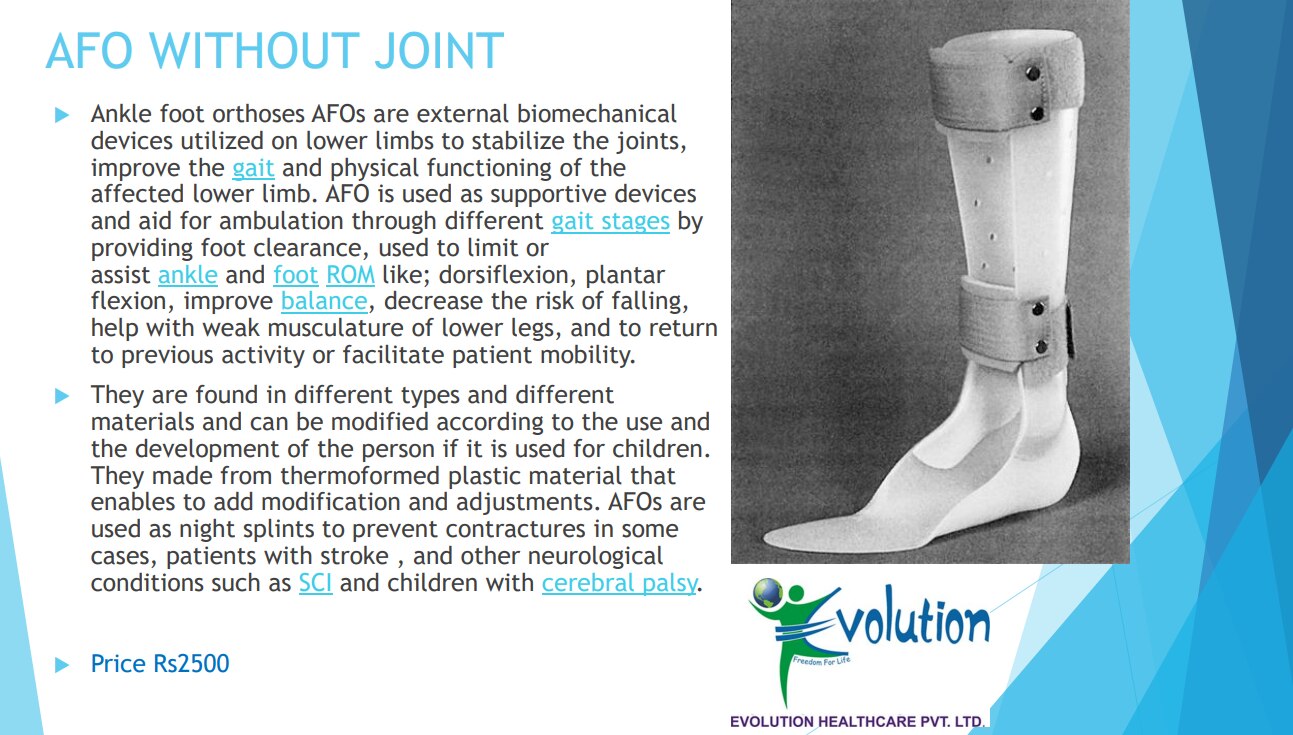
Orthotic Devices: Orthotic devices are supportive braces or splints used to immobilize or support specific body parts during the healing process. They can provide stability and protect joints, muscles, or ligaments. Examples include knee braces, ankle-foot orthoses (AFOs), wrist splints, and back braces.
Range of Motion (ROM) Devices: ROM devices help individuals regain or maintain joint mobility. They can be passive or active. Passive devices, such as continuous passive motion (CPM) machines, move the joints through a controlled range of motion without the individual's effort. Active devices, like pulley systems or therapy bands, require the individual to actively move the joint.
Assistive Devices for Activities of Daily Living (ADL): These aids help individuals perform everyday tasks independently during their rehabilitation. Examples include reachers/grabbers, dressing aids, adaptive utensils, shower chairs, and raised toilet seats.
Electrical Stimulation Devices: Electrical stimulation devices use low-level electrical currents to stimulate nerves and muscles. They can be used to manage pain, prevent muscle atrophy, improve muscle strength, or promote tissue healing.
Balance and Coordination Tools: Balance boards, stability discs, and wobble cushions are aids that help improve balance, coordination, and proprioception.
It's important to note that the specific rehabilitation aids needed may vary depending on the individual's condition, the stage of rehabilitation, and the guidance of healthcare professionals. Consulting with a physiotherapist, occupational therapist, or healthcare provider is crucial to determine the most appropriate rehabilitation aids for an individual's specific needs and goals.
Price: 0 |
Payment Type: |
Available: False |
COD Available: False |
KYC Status:
Send Message